First Peoples' Health and Wellbeing
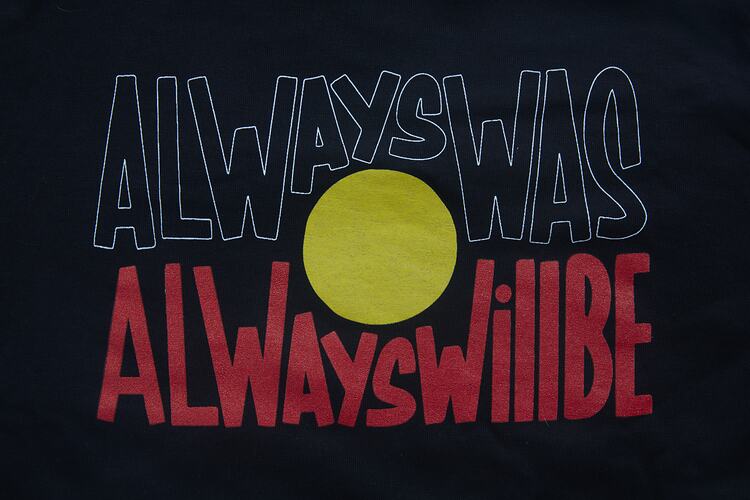
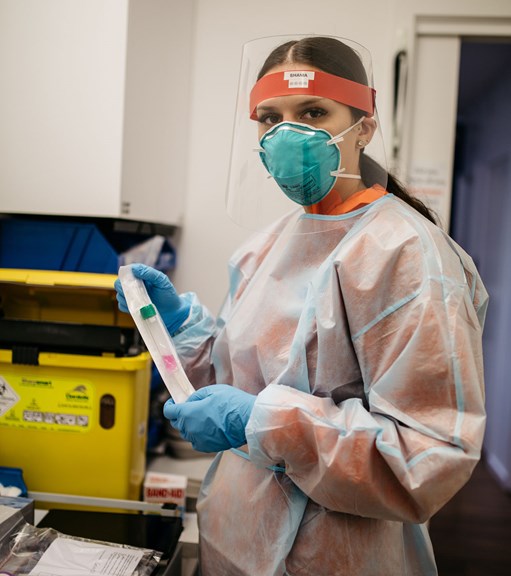
On 11 November 2020, in the middle of NAIDOC week celebrations and in the aftermath of a long period of Stage 4 COVID-19 lockdowns in Victoria, staff members from First Peoples’ Health and Wellbeing (FPHW) posted a video to their social media accounts. This video showed staff dressed in face masks and surgical gowns, peeling down their gowns to expose their T-Shirts made by Aboriginal-owned streetwear label Clothing The Gaps in recognition of the 2020 NAIDOC week theme, ‘Always Was Always Will Be’. The post was accompanied by the words: ‘Fighting COVID together, but we have been fighting for 65,000+ years #alwayswasalwayswillbe #proud #NAIDOC #standstrong.’
In March 2021, proud Taungurung woman and Site Manager of First Peoples’ Health and Wellbeing, Stevie-Lee Ryan, reflected on the impetus behind sharing this video on social media:
‘We just wanted to create an impact, particularly with our Covid respiratory clinic not just being for our Aboriginal and Torres Strait Islander patients, but also for the broader community – just to show that we’re still here, we’re still going strong and we’re looking after everyone as well… I think First Peoples have led the way in their response to COVID-19.’Stevie-Lee Ryan (Taungurung)
First Peoples’ Health and Wellbeing (FPHW) is an Aboriginal community-controlled health service that, along with a number of Aboriginal community-controlled health organisations across Victoria, has played an essential role in delivering culturally safe, holistic primary healthcare to Aboriginal and Torres Strait Islander communities during the COVID-19 pandemic. Prior to the pandemic, FPHW’s Thomastown clinic was opened in 2018 and a second clinic was opened in Frankston in late 2019, both aimed at improving access to affordable primary healthcare for Aboriginal and Torres Strait Islander communities.
When COVID-19 emerged in Victoria and a State of Emergency was declared in March 2020, staff at FPHW worked hard to rapidly transform their Thomastown clinic into a COVID-19 respiratory clinic, becoming one of the first Aboriginal community-controlled respiratory clinics to open in the State of Victoria, with the long-serving Victorian Aboriginal Health Service (VAHS) also establishing a COVID-19 respiratory clinic in Fitzroy. Offering a culturally safe space for Aboriginal and Torres Strait Islander communities to get tested for COVID-19, these respiratory clinics also welcomed non-Indigenous patients.
In March 2021, Museums Victoria curator Catherine Forge visited FPHW’s Thomastown clinic and sat down for an oral history interview with staff members CEO Karinda Taylor (Wamba Wamba), Site Manager Stevie-Lee Ryan (Taungurung) and Medical Administration Officer Shania Shanahan (Arabana). Reflecting on the first year of the pandemic, Karinda, Stevie-Lee and Shania discussed their response to delivering healthcare during COVID-19, including: rapidly setting up a respiratory clinic in Thomastown, increasing staff capacity from 7 to 27 staff members, rolling out a number of flu vaccination clinics, meeting an increased demand for mental health services due to social isolation during lockdown, transitioning in-person appointments to telehealth services, navigating the challenges of being situated in a ‘Covid hot spot’ with positive Covid cases, ensuring staff safety and strict sanitisation procedures at the clinic and preparing for the arrival of the vaccine rollout in 2021.
Beyond their on-site work at the clinic, Karinda, Stevie-Lee and Shania also discussed their wider community outreach work at FPHW, including involvement in NAIDOC week activities, food and hamper deliveries to Elders and community members during lockdown and COVID-19 awareness raising in the Aboriginal and Torres Strait Islander community.
Underlying all this work was a determined focus on closing the gap between Aboriginal and non-Aboriginal people in Australian healthcare, and improving health outcomes for Aboriginal and Torres Strait Islander communities. With a trauma-informed approach to healthcare, staff at FPHW focused their energies in those first 12 months of the pandemic on providing a space where First Peoples patients could feel comfortable and safe; from long consultations over telehealth to extensive community outreach activities that aimed to educate, inform and empower community members through the challenges of COVID-19.
‘We are coming back stronger than ever, and in the middle of a pandemic. We’re not just keeping up with the mainstream, we’re setting the standards in our COVID-19 response.’Karinda Taylor (Wamba Wamba)
The Interview
This interview is based on an abridged / edited version of the oral history interview conducted at the Thomastown clinic on 25 March 2021.
Catherine Forge: We are meeting this afternoon at First Peoples’ Health and Wellbeing in Thomastown on the unceded lands of the Wurundjeri peoples of the Eastern Kulin Nations. Before we begin, I would like to acknowledge the Traditional Owners of the land upon which we are conducting this interview and pay my respects to Elders past, present and emerging. Stevie-Lee, Karinda and Shania, thank you so much for having me here today. To begin, would you like to introduce yourselves?
Karinda Taylor (Wamba Wamba): I’m Karinda Taylor. I’m a Wamba Wamba woman from north-west Victoria and I’m the CEO of First Peoples’ Health and Wellbeing.
Shania Shanahan (Arabana): My name is Shania. I am an Arabana woman and I am a part of the medical and wellbeing team at First Peoples’ Health and Wellbeing Thomastown and studying to be an Aboriginal health practitioner.
Stevie-Lee Ryan (Taungurung): And I’m Stevie-Lee Ryan, a proud Taungurung woman. I am the site manager here at First Peoples’ Health and Wellbeing in Thomastown. Also, I'm a senior Aboriginal health practitioner and a founding member of the organisation.
Catherine: Thank you so much all. Let’s begin at the beginning. Can you tell us a little bit about First Peoples’ Health and Wellbeing?
Karinda: First Peoples’ Health and Wellbeing is a primary health community-controlled Aboriginal health organisation that has been in operation since this Thomastown clinic first opened on the first of November 2018. But the actual organisation’s company name is Access Services for Koories, and we've actually been around since 2010 delivering transportation and care coordination services for chronic disease patients in the community throughout the northern suburbs, so that’s how we landed at Thomastown. We evolved into healthcare due to the increasing Aboriginal population in the northern suburbs and the lack of services. There was a real need in the community to address the gaps in healthcare between Aboriginal and non-Aboriginal people, and provide access to culturally safe, affordable healthcare options for Aboriginal and Torres Straight Islander people.
Stevie-Lee: We also opened a clinic in Frankston in 2019. The 29th of October, so in under a year we opened two clinics. And then we turned into a respiratory clinic in May 2020.
Catherine: Thank you. Let’s talk about that a bit more – what was it like when the pandemic started to arrive?
Stevie-Lee: When the pandemic hadn’t quite hit Australia yet, but we were hearing about the news overseas in Spain in particular, we were actually due to have a team building day which ended up turning into a Covid response day. So, funnily enough, we were down near Melbourne Museum that day and we all sat in the Carlton Gardens and figured out what our response was going to be if COVID-19 hit as hard as it did overseas.
Shania: We were getting prepared for everything. I think we were just trying to plan out what we were going to do, what supplies we would need, PPE and that sort of stuff, because we didn’t know what to expect.
Karinda: The day that we planned this team building day was also the day that Victoria was declared a State of Emergency. We were literally in the gardens behind Melbourne Museum, driving into the city, listening to Dan Andrews talk about the State of Emergency and asking ourselves, “Do we turn around and go home now, or do we come together?” We had a fun day of activities planned including going to museum’s Bunjilaka gallery, and it was suddenly a question of, “what do we do now?” So we took the opportunity to go, “right, what’s our response plan?”, and by the end of that day we had in writing a ten-point response plan that looked at this four-tiered model that just completely upended our entire service.
‘I think the key thing for us was maintaining our warm, kind environment in a world that was literally turned upside down. For example, when the social distancing came into effect, we had to really think deeply about what that meant for our community, and how we could adapt in a way that was in line with our values.’Karinda Taylor (Wamba Wamba)
I think it’s probably the key point of where we tried to stay true to what we do, bearing in mind that we were literally telling people to isolate at home and the northern suburbs for Victoria were probably the hardest hit. It was a hot spot here in Thomastown, so we’ve been at the core of that as a respiratory clinic.
Catherine: I’d love to talk more about this in terms of a core values and the commitment of what you do as an organisation for your community, and how things have had to change with COVID-19.
Karinda: Do you want to talk about our trauma informed approach – the underpinning practices of long consults, and then how we adapted post-COVID-19?
Stevie-Lee: Pre-COVID-19 our structure for seeing patients coming through the clinic was that we have Aboriginal health workers or practitioners or nurses who see patients before they see the GP for their first consult. It’s a 40 minute consult just to allow for that time because we've found that patients would come in with a sore toe, but then would end up opening up about their personal challenges or traumas, because of the way we’ve set up the clinic as calm and welcoming. Our clinic here is not like a usual clinic in terms of being surrounded by medical posters like, “have you got heart disease?”, “have you got diabetes?”
We have intentionally set this clinic up to be warm and welcoming. We've got mob’s artwork on the walls for sale, or just for show. We have our signature lemon myrtle scent so that when patients come in, they can smell that scent and they know where they are. They know they’re safe. We have day spa type music playing in the background to allow for that calming sort of environment, which we've found allows patients to feel comfortable and confident that their confidentiality and privacy is absolutely protected.
‘Then with COVID-19 hitting one of our response points was to look at all of our patients who were on our books and create a plan for them – making sure that they were feeling okay at home, helping them with isolation, making sure that they could get their medications, making sure that we have their pharmacy on file, doing everything that we can to make sure that everyone was feeling safe and okay.’Stevie-Lee Ryan (Taungurung)
And we were actually testing before we became a respiratory clinic, and there was a swab shortage as well at that point, so we were struggling to get PPE, struggling to get swabs, so a big thanks to our CEO who called anyone and everyone, and was able to get a lot of PPE and things that we needed.
Karinda: And we did that with a level of desperation, I think. It’s somewhat easy to look back in hindsight and see where we are now and where broader society has got us to over this 12 month period, but at that point in time there was talk about hospitals being so overwhelmed and so flooded with ICU patients that they would get such a backlog in their emergency departments that ambulances would be paralysed, and that our patients would become our responsibility at end stage of life. That’s the reality. So when we were looking for PPE gear and getting equipment and getting tests, it was a scary time. We even rolled out 12 or 13 flu vaccination clinics – administered over 600 flu vaccinations – which is twenty times more than we've ever done before, because we wanted to ensure that our patients, and particularly our vulnerable patients, were safe.
As Stevie just mentioned, we triaged patients over a certain age, over 70, and then the most vulnerable in terms of chronic disease. We just triaged down and down and down until every single one of our patients got a phone call at some point over the first two or so weeks. It was a huge effort. Everyone was just working around the clock to ensure that we could manage potentially end stage of life requirements at our clinic. It was scary for everybody.
Catherine: Wow. That must have been so much to adapt too, and so quickly too. I’m really interested to hear about community and what their feelings were, how they were responding to your initial work and what was going on in the community?
Shania: So a lot of community who would come and get tested were scared and anxious because other clinics who were doing the testing would go, either really far back at the back of the throat, or really far up the nose where it would hurt or bleed. We are known to be really gentle, so when they would come and get tested with us, we had a lot of feedback and reviews – especially on our Google reviews – saying that we were really gentle, which had a lot of community pretty much come and get tested with us.
Stevie-Lee Ryan: And I think that initially because of Covid, in general everyone was scared. There was an anxiety around the unknown and that feeling of uncertainty that everyone was feeling, you know, “what is this?”, “what’s going to happen to me”? Being isolated from your family, and from community, was a really challenging time for so many people in our community. Pre-Covid we would have Elders who came in here every week and it would be a big day out for them, for connection, so to have that taken away from them during Covid was really hard. Given all the limitations with lockdowns, we absolutely had to adapt. We changed our appointments to primarily telehealth with opportunity for the doctor to triage first, and then if it needed to be a face-to-face discussion, then we would do that on a case-by-case basis depending on the patient’s needs. But in terms of community, it was definitely a very anxious time. You know, people were anxious, and when we did do the phone consults, they went a little bit longer so they had that connection to the outside world and community and mob.
Karinda: It’s been quite an extraordinary 12-month period. I think we’ve gone from seven staff to 27 staff, so rapid growth. We’ve seen a 400% increase in mental health demand too. The fact we’ve been able to build up our new Frankston site during this time – and work remotely with staff that returned to their homes in New South Wales and Western Australia too – is something to be proud of in the midst of a pandemic.
Catherine: Absolutely incredible really. Thinking and talking about staffing, I’m interested to hear about the different roles that each of you have been performing here during the pandemic – your day-to-day work and what that has entailed?
Karinda: I think Shania should go first. She’s got a pretty integral role.
Shania: Okay, I’ll go. So, I started off being in medical admin, working at home for a couple of months I think.
‘And then when we opened the respiratory clinic, I was on the front line of Covid testing every day. So pretty much I would come in, put on the PPE, and then just go out into the carpark and test patients every day.’Shania Shanahan (Arabana)
In the beginning our days were pretty slow, and then when we had our first outbreak it was around 80 to around – I think our most was 100 patients a day. It was scary when we had our first positive Covid case. I really didn’t know what to expect, but it was okay.
Catherine: Was that like a phone call that you got from the health department?
Shania: So, Melbourne Pathology sends the results to us and then when we get these results in our system, we’ll let the doctor know. The doctor will then call the patient to let them know. And then I think a couple of days later they’ll call again just to follow up, the doctor will follow up with the patient to make sure that they’re okay.
Catherine: That must have been terrifying not just for the community, but for staff as well, being on the front line?
Stevie-Lee: I think when we got that first positive case, I remember it coming through at about seven o’clock at night, so my response to that was to ensure that my staff were feeling okay, particularly the ones who were on the front line testing. So I called all the staff, just to check in, see how they were feeling about it, make sure they were feeling okay. And also to ensure that we continued to do our PPE properly and that we shouldn't have anything to worry about. It became very real at that point because we had so many negative tests for a while, and then that first positive was like “oh my God.” But yeah, it was just something that we wanted to support our staff through as well.
Shania: In total we’ve had about 25 positive cases, I think around that.
Karinda: We never lost sight of the fact that we were doing this for our staff and our community, to make sure everyone stayed safe, and that we could respond appropriately, and in a timely manner. I think in my role as the CEO, we’ve got a relatively flat structure, which keeps a level of intimacy, but we do still have a chain of command. Shania has really stepped up during Covid from a more casual medical administration role to being full-time and front-line, as well as doing her Aboriginal health practitioner training, so its’ been a great experience from a clinical perspective. And then of course Stevie, as Site Manager, has made sure that the entire staff has stayed really connected, all while supporting the onboarding of the Site Manager in Frankston, and keeping all the teams connected remotely. My role has involved advocating around the logistics of ongoing PPE and testing. Once we were a GP funded respiratory clinic, things changed a bit and there was an easing of PPE, so it wasn’t as intensive. But it was quite intense at the beginning, working around the clock to chase up PPE and supplies, and making lots of late night phone calls.
Catherine: Thanks for sharing these experiences Shania and Karinda. And what about your role Stevie-Lee?
Stevie-Lee: Yes, my role. So, funny that we mention this, because I was actually appointed the Site Manager role just before Covid hit, so we were essentially cruising along in Thomastown and everything was ready to go in terms of my role and focus as Site Manager of the clinic, and then Covid hit. So when that happened everything had to suddenly change. We split the clinic in half and we still had our primary health Aboriginal health service on one side and then we had our Covid respiratory clinic on the other side. That was pretty rough on staff in terms of how intimate we are and how family orientated we are. To have a wall in between, where we were all looking through a window at each other, was a little bit weird. Everyone felt it.
But yeah, my role entails looking over the whole thing – primary health and the respiratory clinic. At the moment I am trying to sort out the vaccines that have just been released in the last week. We’re still waiting for delivery. I think there’s a shortage going on, so I’m making lots of phone calls to see what’s happening with our order, lots of staff changing rosters and, yeah, just trying to make sure that we can provide that service as well for our community and staff.
Karinda: I think one of the extraordinary things that Stevie has been able to manage in this process is not just the rapid response, but also the significant increase in demand across mental health, which has been largely around the social isolation and the impacts of the restrictions, and what these restrictions mean in terms of potentially re-triggering or traumatising Aboriginal people that have been affected by government policy in the past. This is a real contemporary, modern day example of being re-traumatised. And the fit-out of our clinic is underpinned by a trauma informed space. It’s all done intentionally, so to have that completely flipped by COVID-19, it’s a big change and a big question around how you then manage that.
‘While Covid has been predominantly our focus for the 12 months, we have never lost sight of the complex need around the gaps between Aboriginal and non-Aboriginal people, because these gaps still exist. Covid just got in the way. And in some ways these gaps have probably been exacerbated now. They’re further impacted, so we've got a lot of work to do over the next few years.’Karinda Taylor (Wamba Wamba)
Catherine: Thank you for sharing Karinda. When I was reading your website, I came across this really powerful quote, which said “Australian First Peoples’ culture is the oldest continuing culture on the planet. More than 60,000 years old. To sustain our culture over this time we supported the holistic health of our people through wellbeing and medicine practices handed down through oral traditions.” I was wondering if we could talk a little bit about this from your perspective of working with First Peoples’ Health and Wellbeing?
Karinda: I guess it stems back to where our name came from, so the health and wellbeing component of what we do, and especially the focus on holistic health. This knowledge about holistic health has been passed down from generation to generation, through storytelling and oral traditions, over thousands and thousands of years, over 60,000 years, from the longest living culture in the world. It’s something to be really proud of as Aboriginal people, and that’s why you often hear people say, “I'm a proud Aboriginal woman from” – from wherever their traditional lands are, because our culture and our knowledge systems are something to be really proud of.
What we want do want to in the future is to focus as much on the wellbeing component as the health and broader health component. Some of that will be about the medicinal purposes of traditional bushfoods, so “gukwonderuk”, which is old man weed used for medicinal purposes. Using the lemon myrtle in our clinic is about evoking a safe space for people. Whenever we get Aboriginal catering, we will often get lemon myrtle scones. So at every step of the way we are just trying to incorporate some of that holistic connection. I don’t think we do enough around the bush botanicals yet and we want to do more in that space. We recognise that it’s an important component of the work we do, and that we want to keep exploring this.
‘Our logo is the top of a tea tree plant. I had feedback from a patient who said he came into the clinic and smelt the lemon myrtle scent and it felt like his ancestors were around him and made him feel at home. I'm pretty sure he was from New South Wales, so for him to be somewhere in Victoria on Wurundjeri land and to feel like he is connected and at home is really, really beautiful.’Stevie-Lee Ryan (Taungurung)
Karinda: We’re trying to incorporate the health and wellbeing component at a staffing level too. It’s a little bit more difficult in a western world to incorporate some of that, so it’s a work in progress, but at our staffing level, one of the things that we've really focused on over this last 12 months has been on our staff wellbeing. It became pretty obvious pretty quickly with the rapid response and increase in demand during Covid that at some point something had to give, and it was potentially our staff’s wellbeing. So we took some time out and tried to do some staff development, and one of those things we did was arts therapy with an Aboriginal woman. It was sort of like a meditation with bushfoods, and with tea tree, which is on our logo. There is a lot of evidence about how Aboriginal people used tea tree – as an anti-fungal, anti-inflammatory ointment and for vaporising as well for the lungs. But I think there’s lots more to evolve in that space into the future.
Stevie-Lee: I agree, this is definitely something that we want to focus on a bit more, and bring groups together to do that sort of stuff together. The staff wellbeing sessions were really amazing. We had great feedback about them. It was hard because we were all virtually on Teams, but at least we were all one screen to one person and we had that connection, which I think was really important during the time that we were going through with Covid during the isolation. It sort of brought us all together, especially with all the new faces that were popping up and how quickly our staff were expanding. It was really good.
Catherine: That word connection. I get the sense that connection’s really important not just with your staff, but I feel that perhaps there’s an embedded community kind of connection going on here. Can we talk a little bit about some of the community activities that were going on in the background? I mean we had the Covid testing on one level, but also from what you’ve told me, a lot going on with community?
Stevie-Lee: Yes, so we did some hampers for Christmas. We got a lot of things donated to us as well and then we created hampers to ensure that our patients were – particularly with the big loss of jobs due to Covid – to ensure that our patients had some security around Christmas, with vouchers as well for fresh fruit and vegies and things like that. Frankston did NAIDOC week too and went out to the Gathering Place.
Shania: We did NAIDOC week too, and grazing boxes.
Karinda: We made these grazing boxes and hand-delivered them to people’s homes. It was actually really rewarding and there was lots of feedback from the staff after. As well as that, social media has been a big thing in terms of our community outreach, particularly with our younger audiences. The Tik Toks have been really well received. We've got quite a dynamic young team, haven’t we Shania?
Shania: Yes we do!
Stevie-Lee: Yes, I think with our social media we wanted to create a positive presence as well as keep community informed around the seriousness of Covid.
Catherine: I saw on your website that your mission statement talks about not just the physical wellbeing of an individual, but also the social, emotional and cultural wellbeing of community. I’m interested in what this statement means to you?
Karinda: For me personally, I've got a nursing and midwifery background and the whole reason I went into health was because I lost my grandparents at 52 and 61. My dad at 44, all from preventable disease and lack of access to good primary healthcare that was safe, culturally safe and appropriate and accessible, affordable, and available. All of those things go hand in hand, and that’s why I've entered health, and that’s why I've then come to this organisation. I think that we often talk about connection and collective voice and even at our entire board no one speaks as any one individual – we all have input into everything we do as an organisation.
‘And I think if you’ve got a collective voice heading with a good will and a positive direction around how we will deliver care, you sort of can’t go wrong with that.’Karinda Taylor (Wamba Wamba)
Shania: Yeah, especially with seeing patients as well, they’re not just coming in to have something looked at. In a consultation especially, like Stevie was saying, they come in for one reason and they leave opening up about everything because you give them that space – you let them be vulnerable and open up about everything. I think it’s really important.
Catherine: Absolutely important. I’m wondering on an individual level if any of you would like to perhaps share some of your own personal highlights or challenges of the past 12 months, if you feel comfortable to share?
Shania: For me challenges would be when we first opened up the respiratory clinic, and getting divided into two different teams. That was a challenge for me because I felt like we were isolated away from each other. Red and Green team. But then what made me extremely happy was when we came back all together and I went out doing Covid testing in the car park instead of in the clinic, and the team went kind of back to normal.
Stevie Lee: Um, challenges? Challenges was creating the whole Covid response I suppose! And implementing it. I mean, I'm very, very grateful for the team that we have – and the expertise that everyone has – that was brought together to create what we are and who we are. And being able to provide a high-quality health service to community, because that’s what we want to do.
‘We want to close the health gap. We want to increase the life of Aboriginal people. So, I suppose like that for me is absolutely amazing. The reason why I'm able to do this today is because of my ancestors and what they did for me and I am definitely going to stand up proud and say that we have given everything that we've got, done everything that we can for community.’Stevie-Lee Ryan (Taungurung)
And I suppose one of the hard things for me in the pandemic was not being able to see my mum and my family. Being a Taungurung woman, not being able to go up and have a connection to Country, which I really need. So, that was very, very hard. But I am very thankful for Karinda doing the wellbeing sessions and being able to have that connection with everyone down here. Being able to do the meditation stuff to have the connection with painting and when I did that, I was painting a lot of the Wimmera. Even doing that is not something I would usually paint. Absolutely beautiful. Yeah, I’m very thankful to Karinda and the board for allowing us to have that time to look after ourselves as well as continue to look after community, because without that we’d all probably burn out.
Karinda: I only took on the CEO role six or so months prior to Covid as well, and when I look at my position description and what my job looks like as a CEO and what that entails in a Covid context, it’s been very, very different over these last 12 months. And largely it’s been around creating that support network, but not just me creating that and trying to support others – it’s about these staunch young women here. Covid has made me really just realise how precious people are, and time is, and health and wellbeing more broadly are, and I think the self-care stuff has probably been the stand out for me.
We did self-care packages for all of our staff, and single-handedly went to all these Aboriginal businesses because of course lots of businesses had been completely decimated by Covid. And so to actually go and support 100% Aboriginal businesses and speak to these mostly women running little businesses, boutique ones in their own backyard, during a time when all looks lost, which it did for a bit there during the hardest parts of the lockdown. So not only did we get to support Aboriginal businesses, but we got to hand them to staff and see their faces when they opened these packages that had some gorgeous hand-crafted Aboriginal pieces, and it reminded you that we are a strong, resilient community, and have been for 60,000 plus years.
When you look at Aboriginal Victorian people, we’re back to 50,000 plus, which is what we were over 200 years ago. When you look at how many people we went from and what we got down to, we were all but extinct at that point, and we have come back stronger than ever and in the middle of this pandemic… I think we can thank the Koorie grapevine for that, and our innate need to stay connected as a group.
Catherine: Well, like you say, we’re in the middle of a pandemic, and it’s not over yet, so I want to thank you so much for taking the time in your very busy schedules to sit down and share your knowledge and experiences with me today. And I guess this recording will remain at the museum in our State Collection for future generations, in hundreds of years, to potentially listen to. So, I’m interested to hear what would you want future generations to remember about First Peoples’ Health and Wellbeing and what you’ve been doing here over the pandemic?
Stevie-Lee: That’s a good one. I think just the way that First Peoples have led the way in the response to COVID-19 and our quick response to it as well. Oh, that’s a good question.
'I think the thing to remember for future generations is about remaining true to the core principles of the organisation, so for us around supporting community to stay healthy and strong despite what the challenges are, whether it be externally or internally, and to know that if we stick together, we’ll get through this. The Koorie grapevine is what has kept our Covid numbers low, and it can be nothing else but that. 'Karinda
Shania: We’ve had over 2000 patients, that’s just for our primary health care patients, so Aboriginal and Torres Strait Islander patients, which doesn’t actually include the respiratory clinic patients that we’ve had, so the broader community as well. I think to date we’ve done 6000 Covid tests, so that’s something to be really proud of.
Stevie-Lee: I think the expansion of where we were pre-Covid to now has just been phenomenal in terms of patients. Our delivery of health care and our staffing too, we've done amazing to continue to hold onto who we are and what we are. I’m really proud. I suppose my message to future generations, if First Peoples’ Health and Wellbeing is still around, is to come on board. Follow in our footsteps.
With the Support of the Office for Suburban Development, this oral history interview and accompanying digital photographs have been acquired into Museums Victoria’s State Collection alongside a number of items that were generously donated by First Peoples’ Health and Wellbeing: a FPHW face mask, hand sanitiser, staff T-Shirt, Covid saliva test, medical gown and Clothing the Gap “Always Was Always Will Be” T-Shirt. These items will provide a lasting reminder of the important role of FPHW in delivering Aboriginal-led healthcare and Covid testing during the COVID-19 pandemic.
Museums Victoria acknowledges the many Aboriginal community-controlled health organisations and Aboriginal and Torres Strait Islander health workers that have responded to the COVID-19 pandemic across Victoria and Australia-wide. This story and interview was collected by Catherine Forge in collaboration with Karinda Taylor (Wamba Wamba), Stevie-Lee Ryan (Taungurung) and Shania Shanahan (Arabana).